- My MOC
- Directory
Menu
 10 MIN READ
10 MIN READ
In this article:
As we approach year six of implementation of Competence by Design (CBD), clear signals about the benefits and challenges of the CBD model have emerged from both formal program evaluation and feedback from our invested partner groups. Important challenges include the burden of using Entrustable Professional Activities (EPAs) observations to both frame regular feedback to residents and to assemble data points for resident assessment, time and resources required to implement all aspects of CBD as designed, deploying an electronic learner portfolio, and associated impacts of CBD-related changes on resident and faculty wellness.
It is apparent that our approach to improving education and patient care through the introduction of CBD across Canada has had several unintended negative impacts. While we remain confident in the merits of competency-based medical education (CBME) and are committed to the implementation of related key principles across all specialties, we recognize that a “one size fits all” approach does not consider unique obstacles and opportunities within each local institution, discipline, and program. We also recognize that part of the solution involves addressing barriers of CBD that are at the systems level, outside of the control of individual programs. We trust that postgraduate education leaders will continue delivering quality medical education expected by society if given flexibility to best adapt CBD within the context of their programs.
It is time to refocus efforts on orienting the CBD model to the core principles of CBME intended to improve residency education, while respecting the resources available across institutions and incorporating lessons learned thus far. Multiple invested groups, including the CBD national stakeholder advisory board, have called for increased flexibility of implementation, along with enhanced opportunities for local institutional education leaders to deliver CBD in more efficient ways that match the desired intent of CBD principles with the clinical workflow processes and local context. This document outlines previously existing and new enhanced flexibility for CBD implementation in response to urgent requests for CBD reform. In providing this needed relief from what has been seen by some as an overly rigid system, we must accept that program curriculum design, examination eligibility and certification decisions are all predicated on CBD approaches working effectively in our residency programs. Programs, in partnership with their PGME offices and specialty committees, are encouraged to optimize implementation within their own contexts and resources while maintaining the spirit of the standards articulated by the specialty committees and program directors.
The Essential Requirements of CBD Implementation document is intended to give postgraduate institutions and programs more agency over how they implement specialty-specific standards and CBD document suites, with a distinct focus on easing the burden of assessment that many have experienced. Retaining the principles of increased regular meaningful feedback to learners and enabling confident promotion decisions will require thoughtful integration of EPA observations and other assessment modalities into a coherent system of assessment. With oversight by PGME offices over the implementation of CBD, enhanced flexibility is afforded to programs and their elements in how they reconcile specialty specific requirements within local contexts. Also, we wish to emphasize that Royal College technical guides (e.g., #1 and #3) provide detailed recommendations for high fidelity CBD implementation that are compatible with accreditation standards but are not intended to be absolute requirements.
The Committee on Specialty Education (CSE) has approved The Essential Requirements of CBD Implementation document, effective immediately, which outlines the essential requirements with new enhanced flexibility for program adherence to CBD principles, as reflected in the general and specialty-specific accreditation standards, as well as Royal College policies. Critical requirements for meeting accreditation standards will continue to include:
Accreditation is a holistic evaluation of a program. It is not an evaluation of CBD implementation in isolation. Accreditation seeks to verify that residents have a safe learning environment with appropriate supervision, feedback & coaching, that there is a continuous quality improvement process in place and functioning, that programs are appropriately resourced, and that there are effective leadership and communication processes. The standards and evaluation process focus on the principles of sound educational design. Those involved in the accreditation review and decision-making (surveyors, specialty committees, accreditation committees) seek to verify that the essential requirements for CBD implementation, as outlined above and detailed in the general and specialty-specific standards of accreditation, are in place.
We recognize, however, that it can feel like accreditation puts an undue emphasis on certain components of CBD. We hope this statement helps to clarify for institutions and programs how CBD implementation is approached by surveyors within the accreditation process. In turn, we are committed to ensuring that both volunteers and staff involved in the accreditation process have a clear and renewed understanding of the level of focus and the type and amount of information reviewed, as well as the importance of considering the wider context in which residency training takes place, including factors that impose limitations beyond a program’s control, such as hospital staffing shortages and challenges of poorly functioning electronic systems.
The purpose of this statement is to provide clarity on the enhanced degrees of flexibility in the system and leverages the tremendous efforts of educational champions across the country to build a stronger educational system for residents to thrive in throughout their training. We acknowledge that more formal design adaptations in the CBD model are required to achieve the intended impacts of competency-based medical education, improve the training experience, and address the impact on faculty and residents. With a renewed commitment to action, the Royal College will invest in a national collaborative process over the next 12-18 months to reimagine how CBD can enhance residency training across Canada.
This will involve a series of three Royal College National Summits with key leaders from our invested partner groups to co-create the path forward – the evolution to CBD 2.0.
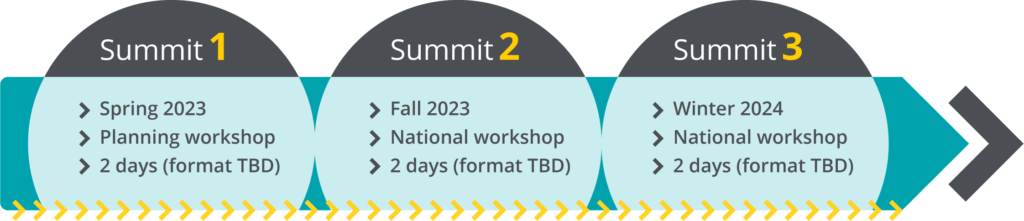
After extensive member checking and opportunities for review from the various invested groups across the country, this collaborative work will then be finalized based on further input and refinement. A final CBD Summit will be held to finalize the national consensus document before submission to the Royal College Committee on Specialty Education (CSE) for decision (Spring 2024). It is hoped initial modifications from the national summits on CBD can begin on July 1, 2024 – with the understanding that some changes to the CBD Framework will occur over a multi-year timeline.
A special thank you to the many groups who contributed their time, expertise and guidance in the collaborative development of this material: the postgraduate deans, National CBME leads, Specialty Committees, Resident Doctors of Canada, Fédération des médecins résidents du Québec, and members of the CBD National Stakeholder Advisory Board, which includes program directors, Specialty Committee chairs, clinician educators, residents and others. We remain committed to the ongoing improvement of the residency training experience for all.
Please direct questions or comments to cbdsecretariat@royalcollege.ca.
Sincerely,
Glen Bandiera, MD, FRCPC, MEd, BASc(Engin)
Executive Director, Office of Standards and Assessment
Royal College
J. Damon Dagnone, MD, FRCPC, MSc, MMEd
Director, Standards and Accreditation
Royal College